Inhala’s comfortable alternative to CPAP that’s FDA-approved Learn about Medicare coverage for Inhala.
Breathe Life In
Medicare recognizes sleep apnea as a serious health condition that requires treatment. At Inhala, we provide the Inhala Oral Appliance, an FDA-approved device that may be covered by Medicare Part B as Durable Medical Equipment (DME).
*With qualifying diagnosis and documentation
Specialists in senior sleep health
Are you experiencing any of these symptoms? Medicare may cover your treatment.
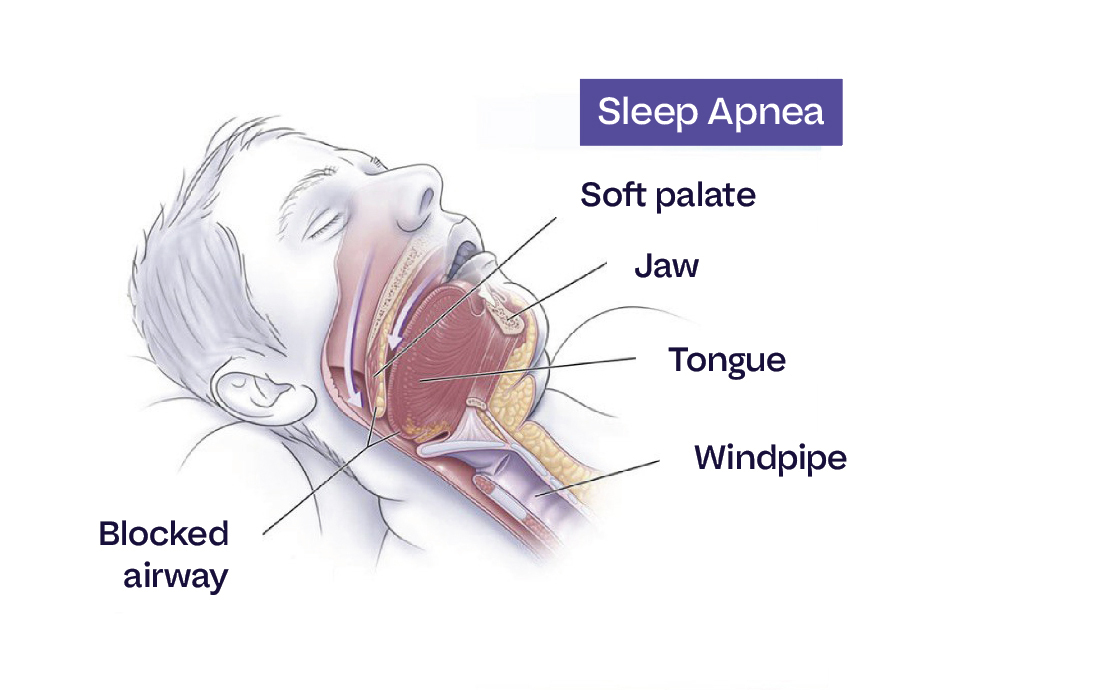
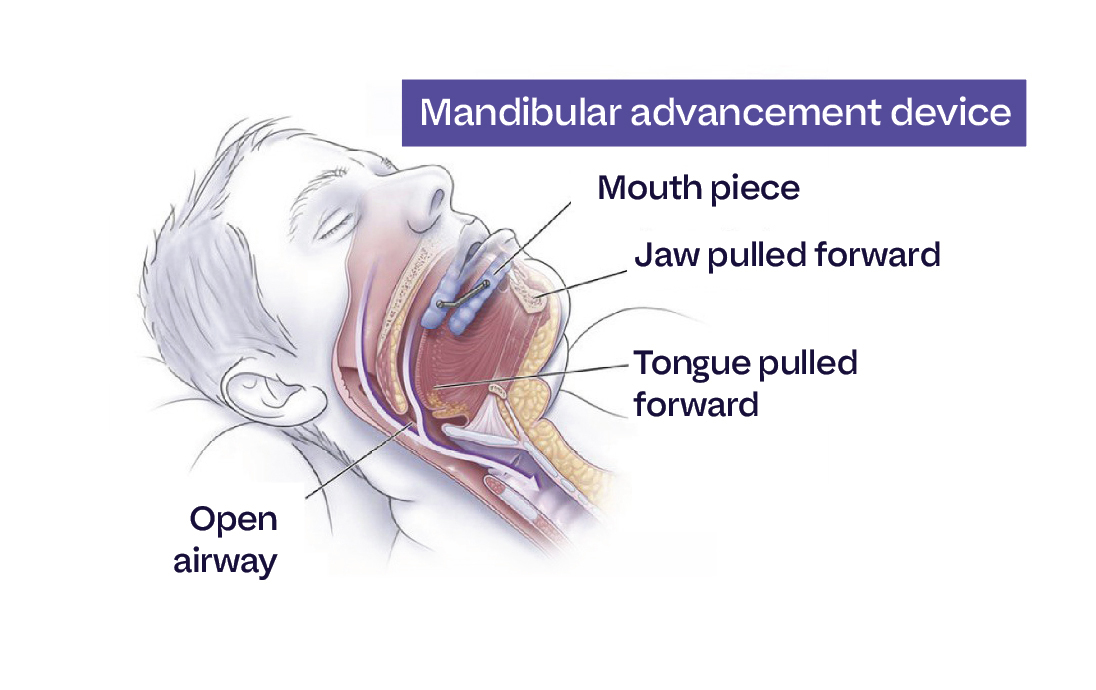
The Inhala Oral Appliance gently repositions your jaw to keep your airway open, providing effective sleep apnea treatment without the noise, mask, or discomfort of CPAP therapy. Inhala’s FDA-Approved custom-fitted device is designed for maximum comfort and effectiveness.
“After struggling with my CPAP for years, I was thrilled when Medicare covered my Inhala Oral Appliance. Now I sleep better than I have in decades thanks to Inhala!” – Margaret P., 72*
* Individual results may vary. Medicare coverage depends on your specific plan and medical necessity.
Medicare Part B covers oral appliance therapy for sleep apnea when:
Enjoy the industry’s only vertically integrated experience. Our team even handles the insurance paperwork for you.


Inhala specializes in treating sleep apnea with comfortable, effective oral appliances. Our team has years of experience working with Medicare patients and handling Medicare claims.
Medicare Part B may cover the Inhala Oral Appliance as Durable Medical Equipment (DME) when:
Coverage is not guaranteed. We’ll help verify your specific benefits.”
Not necessarily. While some patients try CPAP first, Medicare may cover oral appliances as an initial treatment option when medical documentation supports this approach. Coverage requirements vary.
Medicare typically covers 80% of the approved amount. Secondary insurance may cover the remaining costs. Our team will verify your coverage before treatment.
Approval timelines vary based on individual circumstances and Medicare requirements. Our team works to expedite the process when possible.
Yes. We work collaboratively with your physicians to ensure comprehensive care.

Inhala ©2025
For general Medicare coverage information, visit Medicare.gov or call 1-800-MEDICARE.